Discussion on development and maintenance of path of popular science education for cardiopulmonary resuscitation emergency skills
-
+ English摘要:目的
通过观察实时视觉反馈装置对医学生心肺复苏应急技能培养和保持的影响,尝试探讨心肺复苏应急教育科普活动的实施路径。
方法选取2022年6月于南通市第一人民医院临床实习的78名医学生为研究对象(男生33名,女生45名),随机分为实验组和标准组,两组各39人。培训前,对两组的心肺复苏(cardiopulmonary resuscitation,CPR)掌握情况进行考核。接着,标准组在充气人体模型上进行情景模拟心肺复苏技能练习,实验组采用实时视觉反馈设备进行2 min的心肺复苏训练。培训后,依次在四个时间点(第0、10、28和52周)考核两组的理论知识以及操作技能情况,并采用广义估计方程模型比较两组的培训效果。
结果培训前,实验组和标准组学员的基线特征、CPR知识和技能相似,差异无统计学意义(P>0.05),且两组胸部按压的平均深度均未达标。培训后,两组培训效果均有所提升。进一步分析结果显示:(1)实验组第0、10周按压评分高于标准组(P<0.05);两组按压评分从第0周~第28周均有所上升,但在第52周均有所下降(P<0.05)。(2)总体看,培训后高级CPR者占比在实验组、在第28更高(P<0.05)。(3)培训后,标准组胸部按压深度在4个时间点依旧未达标。实验组按压深度在第0、10、28、52周高于标准组(P<0.05),在第10周、28周高于第0周,但在第52周有所下降(P<0.05);标准组第10周按压深度高于第0周,第28周按压评分高于第0周、第10周,但在第52周也有所下降(P<0.05)。(4)培训后,实验组按压频率达到标准,且在第0、10周高于标准组(P<0.05);标准组在第28周、52周按压频率达到标准,且高于第0周、第10周(P<0.05)。(4)培训后,掌握正确的手位及充分的胸部回弹力的学员占比均在实验组更高(P<0.05)。(5)培训后,两组掌握CPR理论知识的学员占比、实施CPR自我认同的学员占比差异均无统计学意义(P>0.05),但总体看,CPR自我认同在第52周时更高(P<0.05)。
结论在心肺复苏术训练中使用实时视觉反馈装置可在短期内提高医学生心肺复苏术技能,并维持较长时间。现代化的培训模式联合传统教学模式能更好地普及并保持医学生高质量心肺复苏的教学成果。
-
我国心搏骤停人数每年高达54.4万人[1],在美国和加拿大,心搏骤停亦是死亡的主要原因[2]。与院外心搏骤停(out-of-hospital cardiac arrest,OHCA)未实施心肺复苏(cardiopulmonary resuscitation,CPR)的病例情况相比,进行规范的CPR可以提高患者的心肺复苏率,从而提高心搏骤停患者的总体生存率[3]。目前,我国43.5% ~ 60%大学生未接受过院前急救培训,其急救理论与技能掌握程度不高[4-5],理解和评估如何有效进行CPR的水平与国外发达国家相差甚远。新时代背景下,高年级医学生作为院外急救的中坚力量,需要也有必要积极进行CPR技能培养。
目前,现代化模拟教育技术的进步带来了各种自动反馈设备。国际复苏联络委员会(International Liaision Committee on Resuscitation,ILCOR)建议在心肺复苏术的培训中使用能够提供指令反馈的设备 [6]。但是,目前少有研究运用当前的CPR指南,探索自动反馈设备在高年级医学生心肺复苏术培训中的应用,也鲜有研究分析医学生进行CPR培训1年后的技能保持情况。
本研究拟以南通市第一人民医院具备基本生命维持(basic life support,BLS)认证的急救医护团队为教学力量,以在该院临床实习的医学生为培训研究对象,采用标准教师指导的CPR心脏按压课程中加入实时视觉反馈装置的教学模式,探索一种适合临床医学生使用并推广的保持高效技能的CPR课程,提升医学院校医学生院前急救能力。
1. 对象与方法
1.1 研究对象
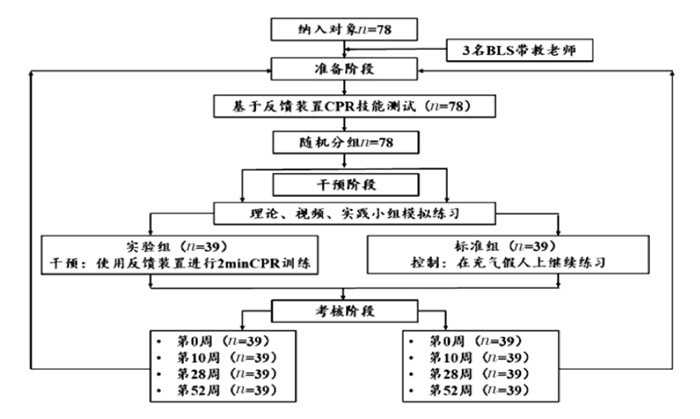
纳入2022年6月于南通市第一人民医院临床实习的78名医学生作为研究对象(不考虑其是否有CPR的经验或培训),其中男生33名,女生45名,涉及专业包括临床医学、影像、口腔、五官、康复。使用在线随机序列发生器(https://www.randomizer.org/)将研究对象随机分为两组:实验组和标准组,每组各39人。为保证培训质量,实践课程由3名BLS认证的医护团队固定开展。本研究经南通市第一人民医院伦理委员会审查批准(伦理编号:2023KT244)。
1.2 方法
1.2.1 路线设计
研究对比了实时视觉反馈设备和情景模拟在培训临床实习医学生心肺复苏技能上的效果,通过考核理论知识和操作技能以及收集学生自我满意度反馈来评估培训成效。2022年6月,学员先集中进行1次全面而系统的培训,学习心肺复苏的理论知识、操作步骤和技巧等,学员们会有一定的时间来消化、吸收和练习所学内容。接着,在2022年6月—2023年6月期间设置4个时间点,进行4次考核来检验学员的学习成果和技能的掌握情况。培训和考核流程见图 1。
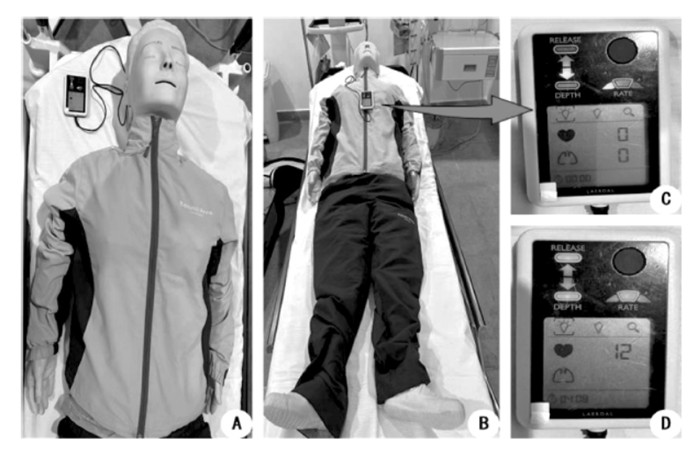
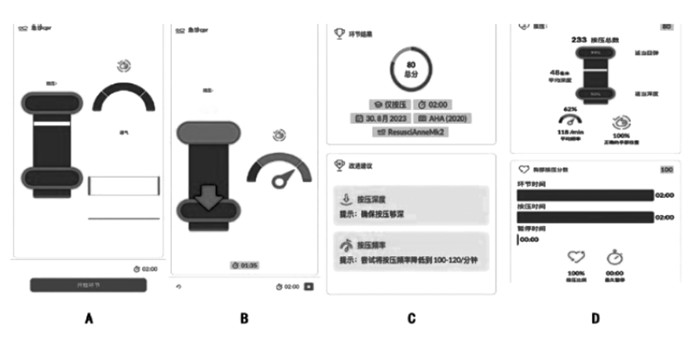
1.2.2 准备阶段
所有研究对象完成1份问卷调查,涉及年龄、性别、培训和实际心肺复苏经验以及CPR基础理论知识。研究对象单独在CPR人体模型Resusci Anne1 QCPR1(美国Laerdal医疗公司)上进行2 min心肺复苏,并重点关注心脏按压。模拟装置通过SkillReporter软件与QCPR应用程序相连,实时反馈按压深度、按压频率、正确的手部位置和充分的胸部回弹力(图 2、图 3)。
1.2.3 干预阶段
准备阶段结束后,研究对象均接受标准的心肺复苏术培训,以《2015版美国心肺复苏指南》《2018中国心肺复苏培训专家共识》为培训内容,使用美国心脏协会(American Heart Association,AHA)认可的“心肺复苏培训套件[7]”,其中包括30 min理论、观摩10 min视频和实践小组模拟练习1 h。
标准组在老师的指导下,围绕教学课程,在充气人体模型上进行情景模拟心肺复苏技能培训,每人在模拟模型上训练3次。实验组在标准组的基础上联合Resusci Anne1 QCPR1人体模型进行2 min CRP心脏按压训练,预先设定成人心肺复苏目标:胸部按压率100 ~ 120次/min,按压深度5 ~ 6 cm [7],同时保证正确的手部位置,充分的胸部回弹。根据学生的实时视觉反馈,采取纠正措施。
1.2.4 考核阶段
在首次干预完成后的第2天到第3天,对两组学生进行测试,研究对象均对反馈人体模型进行2 min的按压CPR,并重点评估其心脏按压关键步骤。两组均完成同一简短的理论问卷,结果记录为第0周的考核成绩。
在测试过程中,仅研究人员可看到成绩,老师和学生均不会收到任何成绩反馈。随后1年内,学生们在干预后的第10周、第28周和第52周被重新评估,其中包括完成1份5个心肺复苏术理论知识的问卷和2 min的CPR心脏按压实操考核。在考核周期内研究对象间无考核内容相关的交流。
1.2.5 观察指标
按压评分(compression score,CS)是由SkillReporter软件根据2015年美国心脏协会成人心肺复苏目标校准的每2 min周期的按压深度、按压频率、正确的手部位置和充分的胸部回弹计算得出的综合评分。QCPR应用程序可直接显示得分[8],满分为100分。
其他指标包括:(1)参与者达到“高级CPR”状态,总体CS ≥ 90分,其中按压评分、开放气道、人工呼吸必须满分;(2)单项关键胸部按压指标满分,如平均按压深度和频率,正确的手位和充分的胸部回弹;(3)理论知识和现实生活中心肺复苏术的自我舒适感,(回答)“是”或“否”;(4)问卷中5个心肺复苏术理论知识题中答对≥ 4题为掌握。
1.2.6 统计学分析
采用SPSS 21.0软件对所整理后的数据进行统计分析。经正态分布检验,服从正态分布的计量资料采用均数±标准差(x ± s)表示,不同时间点的指标采用广义估计方程模型。其中主效应分别为组间及时间,交互效应为组间与时间。服从偏态分布的计量资料采用中位数(四分位数)表示,组间比较采用Mann-Whitney U检验。计数资料采用例数或百分比表示,组间比较采用χ2检验。P < 0.05为差异有统计学意义。
2. 结果
2.1 两组一般资料比较
2022年6月—2023年6月期间,招募78名学生参与者,培训期间没有学生缺席。实验组和标准组的受试者(学员)基线特征、干预前CPR知识和技能相似,且两组学员胸部按压的平均深度均未达标。见表 1。
表 1 两组一般资料情况变量 实验组(n = 39) 标准组(n = 39) t或χ2值 P值 年龄/岁① 22.54 ± 0.64 22.46 ± 0.60 0.546 0.586 性别② 0.053 0.819 男 17(43.6) 16(41.0) 女 22(56.4) 23(59.0) 身高/cm① 168.90 ± 9.59 170.51 ± 9.57 0.745 0.459 体重/kg① 59.36 ± 2.87 59.00 ± 2.60 0.579 0.564 BMI/(kg/m2)① 21.04 ± 2.84 20.50 ± 2.68 0.852 0.397 曾接受CPR培训② 10(25.6) 11(28.2) 0.065 0.799 曾完成真人CPR② 0(0) 1(2.6) < 0.001 > 0.999 BLS老师带教人数② 0.537 0.765 老师A 13(54.2) 11(45.8) 老师B 14(51.9) 13(48.1) 老师C 12(44.4) 15(55.6) 干预前CPR技能① 按压评分 49.46 ± 6.88 49.67 ± 6.28 0.137 0.891 按压深度/mm 34.23 ± 3.82 35.46 ± 3.10 1.562 0.123 按压频率/min 109.08 ± 10.04 109.82 ± 11.74 0.301 0.765 正确的手位② 9(23.1) 8(20.5) 0.075 0.784 充分的胸部回弹力② 8(20.5) 9(23.1) 0.075 0.784 掌握CPR理论知识② 17(43.6) 16(41.0) 0.053 0.819 CPR的自我认可② 3(7.7) 4(10.3) < 0.001 > 0.999 注:①以(x ± s)表示;②以[例数(占比/%)]表示。 2.2 按压评分(CS)和高级心肺复苏术者
培训后,两组培训效果均有所提升。故进一步采用广义估计方程模型比较两组在不同时间点的培训效果。广义估计方程模型中,比较胸部按压评分差异采用的连接函数为线性回归。模型效应检验结果显示:按压得分在两组间差异有统计学意义,在不同时间差异也有统计学意义,且时间和组间存在交互作用(P < 0.05)。进一步进行单独效应分析,其中组间比较:实验组第0、10周按压评分高于标准组(P < 0.05);不同时间点比较,实验组第10周、28周按压评分高于第0周,第52周按压评分高于第0、10周,但低于第28周(P < 0.05);标准组第10周按压评分高于第0周,第28周按压评分高于第0、10周,第52周按压评分高于第0周,但低于第28周(P < 0.05)。可见两组按压评分从第0周~ 第28周均有所上升,但在第52周均有所下降(P < 0.05)。见表 2。
表 2 两组按压评分(CS)和高级心肺复苏术者比较组别 例数 按压评分① 高级CPR者② 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 70.44 ± 6.84③ 89.23 ± 7.89③ 92.72 ± 5.74③ 79.97 ± 8.94 25(64.1)③ 32(82.1)③ 36(92.3)③ 31(79.5) 标准组 39 60.00 ± 7.18 80.31 ± 5.23 89.26 ± 6.51 78.56 ± 5.92 16(41.0) 24(61.5) 29(74.4) 27(69.2) Wald χ组间2,P组间 55.642, < 0.001 10.419, < 0.001 Wald χ时间2,P时间 573.714, < 0.001 21.360, < 0.001 Wald χ交互2,P交互 22.284, < 0.001 1.448,0.694 注:①以(x ± s)表示;②以[例数(占比/%)]表示;③与标准组同时间点比较,P < 0.05。 比较高级CPR者占比差异采用的连接函数为logistic回归。模型效应检验结果显示:高级CPR者占比在两组间差异有统计学意义,在不同时间点差异也有统计学意义(P < 0.05),但时间和组间不存在交互作用。故仅分析主效应,结果显示:不考虑时间,高级CPR者占比在实验组更高;不考虑组别,高级CPR者占比在第28周更高(P < 0.05)。见表 2。
2.3 关键胸部按压指标
培训后,标准组胸部按压深度在4个时间点依旧未达标。进一步的广义估计方程模型分析中,比较按压深度差异采用的连接函数为线性回归。模型效应检验结果显示:按压深度在两组间差异有统计学意义,在不同时间差异也有统计学意义,且时间和组间存在交互作用(P < 0.05)。进一步进行单独效应分析,其中组间比较:实验组第0、10、28、52周按压深度高于标准组,差异有统计学意义(P < 0.05)。不同时间点比较,实验组第10、28周按压深度高于第0周,第52周按压深度低于第0周、第10周、第28周(P < 0.05);标准组第10周按压深度高于第0周,第28周按压评分高于第0、10周,第52周按压深度低于第10、28周(P < 0.05)。
培训后,实验组按压频率达到标准。进一步的广义估计方程模型分析中,比较按压频率差异采用的连接函数为线性回归。模型效应检验结果显示:按压频率在两组间差异有统计学意义,在不同时间差异也有统计学意义,且时间和组间存在交互作用(P < 0.05)。进一步进行单独效应分析,其中组间比较:实验组第0、10周按压频率高于标准组,差异有统计学意义(P < 0.05)。不同时间点比较,实验组第52周按压频率低于第0周(P < 0.05);标准组第28、52周按压频率高于第0、10周(P < 0.05)。
比较掌握正确手位的学员占比差异采用的连接函数为logistic回归。模型效应检验结果显示:掌握正确手位的人员占比在两组间差异有统计学意义(P < 0.05),在不同时间差异无统计学意义,且时间和组间不存在交互作用。故仅分析主效应,结果显示,不考虑时间因素,掌握正确手位的人员占比在实验组更高(P < 0.05)。
比较掌握充分的胸部回弹力的学员占比差异采用的连接函数为logistic回归。模型效应检验结果显示:掌握充分的胸部回弹力的学员占比在两组间差异有统计学意义(P < 0.05),但在不同时间点差异无统计学意义,且时间和组间不存在交互作用。故仅分析主效应,结果显示,不考虑时间因素,掌握充分的胸部回弹力的学员占比在实验组更高(P < 0.05)。详见表 3。
表 3 两组CPR关键胸部按压指标比较组别 例数 按压深度②/mm 按压频率②/min 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 49.36 ± 2.67① 54.61 ± 4.36① 53.97 ± 3.54① 47.38 ± 2.94① 115.03 ± 6.97① 110.13 ± 6.94① 112.15 ± 9.27 106.87 ± 7.60 标准组 39 41.21 ± 2.64 45.62 ± 4.20 49.92 ± 3.93 39.31 ± 4.25 98.90 ± 6.63 99.69 ± 8.91 109.21 ± 5.70 109.85 ± 8.52 Wald χ组间2,P组间 353.761, < 0.001 49.670, < 0.001 Wald χ时间2,P时间 269.889, < 0.001 27.881, < 0.001 Wald χ交互2,P交互 22.926, < 0.001 88.238, < 0.001 组别 例数 正确的手位③ 充分的胸部回弹力③ 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 35(89.7)① 34(87.2)① 32(82.1) 30(76.9) 32(82.1)① 32(82.1)① 33(84.6) 33(84.6) 标准组 39 28(71.8) 26(66.7) 25(64.1) 24(6.15) 23(59.0) 24(61.5) 28(71.8) 31(79.5) Wald χ组间2,P组间 14.247, < 0.001 8.222,0.004 Wald χ时间2,P时间 3.453,0.327 2.117,0.548 Wald χ交互2,P交互 0.566,0.904 0.905,0.824 注: ①与标准组同时间点比较,P < 0.05;②以(x ± s)表示;③以[例数(占比/%)]表示。 2.4 心肺复苏术知识和在现实生活中执行心肺复苏术的自信心
比较掌握CPR理论知识的学员占比差异采用的连接函数为logistic回归。模型效应检验结果显示:掌握CPR理论知识在两组间差异无统计学意义,在不同时间差异也无统计学意义,时间和组间不存在交互作用。
比较实施CPR自我认同的学员占比差异采用的连接函数为logistic回归。模型效应检验结果显示:实施CPR自我认同在两组间差异无统计学意义,在不同时间点差异有统计学意义(P < 0.05),但时间和组间不存在交互作用。故仅分析时间主效应,结果显示,不考虑组别因素,实施CPR自我认同的学员占比在第52周更高。详见表 4。
表 4 两组理论知识和心肺复苏术的自我感舒度比较[例数(占比/%)] 组别 例数 掌握CPR理论知识 实施CPR自我认同 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 29(74.4) 34(87.2) 35(89.7) 34(87.2) 16(41.0) 27(69.2) 31(79.5) 34(87.2) 标准组 39 30(76.9) 33(84.6) 34(87.2) 35(89.7) 17(43.6) 28(71.8) 31(79.5) 31(79.5) Wald χ组间2,P组间 0.002,0.961 0.095,0.757 Wald χ时间2,P时间 5.334,0.149 34.995, < 0.001 Wald χ交互2,P交互 0.380,0.944 1.037,0.792 3. 讨论
研究表明,旁观者主动实施心肺复苏能在一定程度上改善心搏骤停患者的生存结果,但由于实施者缺乏急救知识,或心理负担过重,容易导致抢救不及时,最终错过黄金急救期[9]。心肺复苏训练是医学生的必备技能,Sullivan等[10]建议,心肺复苏培训要定期加强以按压和通气质量为重点的练习课程。既往文献[11-14]研究了不同的教育方法,包括科普宣传、线上线下结合、基于视频和虚拟现实培训、电子学习模块的推广等,均能不同程度地提高培训成果。但如何有效地开展心肺复苏培训,高质量地达到心肺复苏培训中定性或定量的要求[15],通过高效率运用反馈装置从而较大程度保持培训效果是本研究重点关注的内容。
本次调查结果显示,在培训前,两组学员胸部按压的平均深度均未达标,且CPR知识和技能掌握情况不佳。培训后,两组培训效果均有所提升,但标准组的胸部按压深度依旧不达标。而实验组的按压深度和频率更符合规定的标准范围,且在按压评分、高级CPR者占比等各项指标中,实验组在4个时间点的大部分表现都好于标准组,说明心肺复苏训练结合实时视觉反馈能显著提高培训技能。这与王静等[16]的结论一致,前者进行了3轮为期5 d的短期技能强化训练,而本研究培训和考核周期历时1年,更注重知识的系统性和实践能力的全面提升。Sutton等[17]指出,在6个月的时间内提供4次短期培训后,65%的参与者的心肺复苏技能表现有所改善。Sullivan等[10]认为每隔6个月进行培训的效果没有每隔3个月的成绩显著。本研究对研究对象培训后的技能保持情况进行分析,发现在心肺复苏术培训中使用反馈设备的益处可长达28周。提示学员们者不仅掌握了基本技巧,而且在实践应用中技能得到巩固,具备了更高的熟练度和自信心。
另外,本次研究也发现,随着时间的延长,两组按压频率、按压手位以及充分的胸部回弹等指标的差异在培训后的第28周开始缩小,同时按压评分、高级CPR者占比以及按压深度的差异在第52周缩小。这提示,在第28周引入培训课程可以更大程度地保持技能的肌肉记忆。知识和技能的保持是心肺复苏术培训成功的关键,在今后的教学中应根据学生的不同情况,制定出适宜的培训方案,尤其要在第28周注重技能损失,及时进行重复记忆训练。
与基线相比,两种心肺复苏培训方法都能提高学生的理论知识,及其在现实生活中进行心肺复苏术的自我认同。Wingen等[18]也报道了18 ~ 22岁学生在培训后6个月的知识和自信水平方面的类似结果。在12.5 ~ 14.5岁的学龄儿童中进行心肺复苏术培训对帮助他人的态度和意愿有益[19]。心肺复苏能力的自我认同是现实生活中心肺复苏术实施者的强大独立预测因素[20]。
本次研究有几点局限性:首先,本研究是在地市级某一家三甲教学医院中进行的,得出的结论可能无法适用其他教学医院,今后将联合多家教学医院开展多中心研究。其次,研究中带教老师和研究参与者不能进行反馈干预,如果学生在每次简短的后续访问中接受实时反馈,其技能可能能够保持更久。第三,由于时间限制,在实验组中每个学生只能进行2 min的反馈装置训练。拉长训练时间可使学生练习关键技能,接受指导性反馈、改进表现直到掌握为止。
总之,在心肺复苏术培训中使用实时视觉反馈装置短期内可显著提高医学生心肺复苏术技能掌握程度,而任何技能保持的核心都是“低剂量、高频率”的复习训练。信息技术高速发展的今天,现代化的培训模式联合传统教学模式才能满足时代需求,教学过程中应充分结合医学生的个性化发展需求,才能更好地普及并保持医学生高质量心肺复苏的教学成果。
作者声明 本文无实际或潜在的利益冲突 -
表 1 两组一般资料情况
变量 实验组(n = 39) 标准组(n = 39) t或χ2值 P值 年龄/岁① 22.54 ± 0.64 22.46 ± 0.60 0.546 0.586 性别② 0.053 0.819 男 17(43.6) 16(41.0) 女 22(56.4) 23(59.0) 身高/cm① 168.90 ± 9.59 170.51 ± 9.57 0.745 0.459 体重/kg① 59.36 ± 2.87 59.00 ± 2.60 0.579 0.564 BMI/(kg/m2)① 21.04 ± 2.84 20.50 ± 2.68 0.852 0.397 曾接受CPR培训② 10(25.6) 11(28.2) 0.065 0.799 曾完成真人CPR② 0(0) 1(2.6) < 0.001 > 0.999 BLS老师带教人数② 0.537 0.765 老师A 13(54.2) 11(45.8) 老师B 14(51.9) 13(48.1) 老师C 12(44.4) 15(55.6) 干预前CPR技能① 按压评分 49.46 ± 6.88 49.67 ± 6.28 0.137 0.891 按压深度/mm 34.23 ± 3.82 35.46 ± 3.10 1.562 0.123 按压频率/min 109.08 ± 10.04 109.82 ± 11.74 0.301 0.765 正确的手位② 9(23.1) 8(20.5) 0.075 0.784 充分的胸部回弹力② 8(20.5) 9(23.1) 0.075 0.784 掌握CPR理论知识② 17(43.6) 16(41.0) 0.053 0.819 CPR的自我认可② 3(7.7) 4(10.3) < 0.001 > 0.999 注:①以(x ± s)表示;②以[例数(占比/%)]表示。 表 2 两组按压评分(CS)和高级心肺复苏术者比较
组别 例数 按压评分① 高级CPR者② 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 70.44 ± 6.84③ 89.23 ± 7.89③ 92.72 ± 5.74③ 79.97 ± 8.94 25(64.1)③ 32(82.1)③ 36(92.3)③ 31(79.5) 标准组 39 60.00 ± 7.18 80.31 ± 5.23 89.26 ± 6.51 78.56 ± 5.92 16(41.0) 24(61.5) 29(74.4) 27(69.2) Wald χ组间2,P组间 55.642, < 0.001 10.419, < 0.001 Wald χ时间2,P时间 573.714, < 0.001 21.360, < 0.001 Wald χ交互2,P交互 22.284, < 0.001 1.448,0.694 注:①以(x ± s)表示;②以[例数(占比/%)]表示;③与标准组同时间点比较,P < 0.05。 表 3 两组CPR关键胸部按压指标比较
组别 例数 按压深度②/mm 按压频率②/min 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 49.36 ± 2.67① 54.61 ± 4.36① 53.97 ± 3.54① 47.38 ± 2.94① 115.03 ± 6.97① 110.13 ± 6.94① 112.15 ± 9.27 106.87 ± 7.60 标准组 39 41.21 ± 2.64 45.62 ± 4.20 49.92 ± 3.93 39.31 ± 4.25 98.90 ± 6.63 99.69 ± 8.91 109.21 ± 5.70 109.85 ± 8.52 Wald χ组间2,P组间 353.761, < 0.001 49.670, < 0.001 Wald χ时间2,P时间 269.889, < 0.001 27.881, < 0.001 Wald χ交互2,P交互 22.926, < 0.001 88.238, < 0.001 组别 例数 正确的手位③ 充分的胸部回弹力③ 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 35(89.7)① 34(87.2)① 32(82.1) 30(76.9) 32(82.1)① 32(82.1)① 33(84.6) 33(84.6) 标准组 39 28(71.8) 26(66.7) 25(64.1) 24(6.15) 23(59.0) 24(61.5) 28(71.8) 31(79.5) Wald χ组间2,P组间 14.247, < 0.001 8.222,0.004 Wald χ时间2,P时间 3.453,0.327 2.117,0.548 Wald χ交互2,P交互 0.566,0.904 0.905,0.824 注: ①与标准组同时间点比较,P < 0.05;②以(x ± s)表示;③以[例数(占比/%)]表示。 表 4 两组理论知识和心肺复苏术的自我感舒度比较
[例数(占比/%)] 组别 例数 掌握CPR理论知识 实施CPR自我认同 第0周 第10周 第28周 第52周 第0周 第10周 第28周 第52周 实验组 39 29(74.4) 34(87.2) 35(89.7) 34(87.2) 16(41.0) 27(69.2) 31(79.5) 34(87.2) 标准组 39 30(76.9) 33(84.6) 34(87.2) 35(89.7) 17(43.6) 28(71.8) 31(79.5) 31(79.5) Wald χ组间2,P组间 0.002,0.961 0.095,0.757 Wald χ时间2,P时间 5.334,0.149 34.995, < 0.001 Wald χ交互2,P交互 0.380,0.944 1.037,0.792 -
[1] YAN S J, GANY, WANG R X, et al. Willingness to attend cardiopulmonary resuscitation training and the associated factors among adults in China[J]. Crit Care, 2020, 24(1): 457. doi: 10.1186/s13054-020-03165-1
[2] BERDOWSKI J, BERG R A, TIJSSEN J G, et al. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies[J]. Resuscitation, 2010, 81(11): 1479-1487. doi: 10.1016/j.resuscitation.2010.08.006
[3] JENTZER J C, CLEMENTS C M, MURPHY J G, et al. Recent developments in the management of patients resuscitated from cardiac arrest[J]. J Crit Care, 2017, 39: 97-107. doi: 10.1016/j.jcrc.2017.02.011
[4] 赵俊, 鞠丹, 黄玲, 等. 某大学学生对心肺复苏术的认知现状调查及对策探讨[J]. 中华危重病急救医学, 2013, 25(2): 121-122. [5] 杨凡, 马青变. 2020年心肺复苏领域研究进展[J]. 中国急救医学, 2021, 41(7): 593-595. doi: 10.3969/j.issn.1002-1949.2021.07.011 [6] BALDI E, CORNARA S, CONTRI E, et al. Real-time visual feedback during training improves laypersons' CPR quality: a randomized controlled manikin study[J]. CJEM, 2017, 19(6): 480-487. doi: 10.1017/cem.2016.410
[7] American Heart Association. CPR and first aid emergency cardiovascular care, CPR in schools training kits[EB/OL]. (2020-02-02)[2023-08-30]. https://cpr.heart.org/en/courses/cpr-in-schools-training-kits.
[8] LAERDAL. CPR scoring explained[EB/OL]. (2019-06-20)[2023-08-30]. http://cdn.laerdal.com/downloadstest/f3784/Att_2_to_000-21778.pdf.
[9] 张文武, 梁锦峰, 窦清理, 等. 社会急救培训体系建设与实践[J]. 中国急救医学, 2022, 42(10): 829-833. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJJY202210001.htm [10] SULLIVAN N J, DUVAL-ARNOULD J, TWILLEY M, et al. Simulation exercise to improve retention of cardiopulmonary resuscitation priorities for in-hospital cardiac arrests: a randomized controlled trial [J]. Resuscitation, 2015, 86: 6-13. doi: 10.1016/j.resuscitation.2014.10.021
[11] WANG R, HAN J, LIU C, et al. Relationship between medical students' perceived instructor role and their approaches to using online learning technologies in a cloud-based virtual classroom[J]. BMC Med Educ, 2022, 22(1): 560. doi: 10.1186/s12909-022-03604-3
[12] 罗仕琦, 冯志坚, 郑帅, 等. MOOC与云课堂混合式教学模式在内科学教学中的应用研究[J]. 中国继续医学教育, 2022, 14(12): 44-47. doi: 10.3969/j.issn.1674-9308.2022.12.012 [13] 樊冰. 基于云课堂的混合式教学模式在影像设备学教学中的应用[J]. 中国中医药现代远程教育, 2022, 20(14): 21-23. doi: 10.3969/j.issn.1672-2779.2022.14.008 [14] 封彬, 高文慧, 徐佳丽, 等. 多模式教学在高职学生心肺复苏技能培训中的应用[J]. 中国急救复苏与灾害医学杂志, 2023, 18(1): 117-120. doi: 10.3969/j.issn.1673-6966.2023.01.029 [15] 中国研究型医院学会心肺复苏学专业委员会中华医学会科学普及分会. 2018中国心肺复苏培训专家共识[J]. 中华危重病急救医学, 2018, 30(5): 385-400. doi: 10.3760/cma.j.issn.2095-4352.2018.05.001 [16] 王静, 金晓晴, 刘瑞宁, 等. 强化训练联合实时反馈装置的CPR培训对教学效果影响的研究[J]. 中华急诊医学杂志, 2019, 28(2): 199-202. [17] SUTTON R M, NILES D, MEANEY P A, et al. Low-dose, highfrequency CPR training improves skill retention of in-hospital pediatric providers[J]. Pediatrics, 2011, 128(1): e145-e151. doi: 10.1542/peds.2010-2105
[18] WINGEN S, SCHROEDER D C, ECKER H, et al. Selfconfidence and level of knowledge after cardiopulmonary resuscitation training in14 to 18 year old schoolchildren: a randomised-interventional controlled study in secondary schools in Germany[J]. Eur J Anaesthesiol, 2018, 35(7): 519-526. doi: 10.1097/EJA.0000000000000766
[19] PIVAC S, GRADISEK P, SKELA-SAVIC B. The impact of cardiopulmonary resuscitation (CPR) training on schoolchildren and their CPR knowledge, attitudes toward CPR, and willingness to help others and to perform CPR: mixed methods research design[J]. BMC Public Health, 2020, 20(1): 915. doi: 10.1186/s12889-020-09072-y
[20] LU C, JIN Y H, SHI X T, et al. Factors influencing Chinese university students' willingness to performing bystander cardiopulmonary resuscitation[J]. Int Emerg Nurs, 2017, 32: 3-8. doi: 10.1016/j.ienj.2016.04.001




 下载:
下载: